| This article or section is in the middle of an expansion or major restructuring. You are welcome to assist in its construction by editing it as well. If this article has not been edited in several days, please remove this template. This article was last edited by Mallexikon (talk | contribs) 20 seconds' time. (Purge) |
| | The neutrality of this article is disputed. Please see the discussion on the talk page. Please do not remove this message until the dispute is resolved. (March 2011) |
| This article needs additional citations for verification. Please help improve this article by adding reliable references. Unsourced material may be challenged and removed. (March 2011) |
Traditional Chinese medicine (中醫, pinyin: zhōng yī) (TCM), is a label that covers a broad range of traditional medicine practices spread throughout Asia, including various forms of herbal medicine, acupuncture, massage therapy, and dietary therapy.[1] The common thread among these diverse practices is a system for balancing the various functions of the body, based in Daoist principles of yinyang and other metaphysical belief systems, that originated during the Warring States Period in regions that are now part of China. These practices are a common part of medical care throughout East Asia, accounting for roughly 75% of worldwide use,[2][3] but are considered alternative medicine in the western world.[1]
TCM practices use a different physiological model than modern medicine, and make a number of assumptions that are inconsistent with or untestable under the principles of scientific methods. In general, TCM practices take a holistic approach, viewing the body in terms of organ system based loosely around particular body functions (such as digestion or excretion) rather than in terms of isolated organs. These organ systems are conceived to be interrelated in various systematic ways, and various techniques are used to stimulate or support weakened systems or to soothe or dampen over-excited systems. TCM involves an often subjective diagnosis of the general state of various organ systems followed by ongoing efforts to reestablish a healthy balance between the systems. There is no scientific evidence for these theories of medicine.
A broad range of 'over-the-counter' medicinals loosely related to TCM are available. Many of these - such as yinchiao, a commonly used medicinal for colds and flus - are innocuous, but some may contain dangerous chemicals added as ingredients or byproducts of production, and certain sexual potency medicinals are complicit in the near extinction of animals such as the rhinoceros and siberian tiger.
TCM is not based on modern anatomical and disease models, complicating research on the efficacy of TCM medicinals and practices. Interpretation of studies of the efficacy of acupuncture remains controversial due largely to questions of designing an effective placebo.
Contents1 Philosophical background |
[edit] Philosophical background
Traditional Chinese Medicine (TCM) is based on Yinyangism (i.e., the combination of Five Phases theory with Yin-yang theory),[4] which was later absorbed by Daoism.[5]
[edit] Yin and yang
Yin and yang are ancient Chinese concepts which can be traced back to the Shang dynasty[6] (1600-1100 BC). They represent two abstract[7] and complimentary aspects every phenomenon in the universe can be divided into.[6] Primordial analogies for these aspects are the sun-facing (yang) and the shady (yin) side of a hill.[8] Two other commonly used representational allegories of yin and yang are water and fire.[7] In yin-yang theory, detailed attributions are made regarding the yin or yang character of things:
| Phenomenon | Yin | Yang |
|---|---|---|
| Celestial bodies[9] | moon | sun |
| Gender[9] | female | male |
| Location[9] | inside | outside |
| Temperature[9] | cold | hot |
| Direction[10] | downward | upward |
| Degree of humidity | damp/moist | dry |
The concept of yin and yang is also applicable to the human body; for example, the upper part of the body and the back are assigned to yang, while the lower part of the body are believed to have yin character.[11] Yin and yang characterization also extends to the various body functions, and - more importantly - to disease symptoms (e.g., cold and heat sensations are assumed to be yin and yang symptoms, respectively).[10] Thus, yin and yang of the body are seen as phenomena whose lack (or overabundance) comes with characteristic symptom combinations:
- Yin vacuity (also termed "vacuity-heat"): heat sensations, possible night sweats, insomnia, dry pharynx, dry mouth, dark urine, a red tongue with scant fur, and a "fine" and rapid pulse.[12]
- Yang vacuity ("vacuity-cold"): aversion to cold, cold limbs, bright white complexion, long voidings of clear urine, diarrhea, pale and enlarged tongue, and a slightly weak, slow and fine pulse.[13]
TCM also identifies drugs believed to treat these specific symptom combinations, i.e., to reinforce yin and yang.[14]
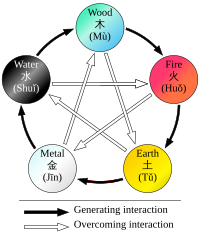
[edit] Five Phases theory
Five Phases (五行, pinyin: wǔ xíng, sometimes also translated as "Five Elements")[15] theory presumes that all phenomena of the universe and of nature can be broken down into five elemental qualities - represented by wood (木, pinyin: mù), fire (火pinyin: huǒ), earth (土, pinyin: tǔ), metal (金, pinyin: jīn), and water (水, pinyin: shuǐ).[16] In this way, lines of correspondence can be drawn:
| Phenomenon | Wood | Fire | Earth | Metal | Water |
|---|---|---|---|---|---|
| Direction[17] | east | south | center | west | north |
| Color[18] | green/blue | red | yellow | white | black |
| Climate[17] | wind | heat | damp | dryness | cold |
| Taste[19] | sour | bitter | sweet | acrid | salty |
| Sense organ[20] | eye | tongue | mouth | nose | ears |
| Facial part[21] | above bridge of nose | between eyes, lower part | bridge of nose | between eyes, middle part | cheeks (below cheekbone) |
| Eye part[22] | iris | inner/outer corner of the eye | upper and lower lid | sclera | pupil |
Strict rules are identified to apply to the relationships between the Five Phases in terms of sequence, of acting on each other, of counteraction etc.[16] All these aspects of Five Phases theory constitute the basis of the zàng-fǔ concept, and thus have great influence regarding the TCM model of the body.[15] Five Phase theory is also applied in diagnosis and therapy.[15]
Correspondences between the body and the universe have historically not only been seen in terms of the Five Elements, but also of the "Great Numbers" (大數, pinyin: dà shū)[23] For example, the number of acupoints has at times been seen to be 365, in correspondence with the number of days in a year; and the number of main meridians - 12 - has been seen in correspondence with the number of rivers flowing through the ancient Chinese empire.[24][25]
[edit] TCM model of the body
| | The following text needs to be harmonized with text in TCM model of the body. |
TCM's view of the human body is only marginally concerned with anatomical structures, but focuses primarily on the body's functions[26][27] (such as digestion, breathing, temperature maintenance, etc.):
"The tendency of Chinese thought is to seek out dynamic functional activity rather than to look for the fixed somatic structures that perform the activities. Because of this, the Chinese have no system of anatomy comparable to that of the West."
—Ted Kaptchuck, The Web That Has No Weaver
These functions are aggregated and then associated with a primary functional entity - for instance, nourishment of the tissues and maintenance of their moisture are seen as connected functions, and the entity postulated to be responsible for these functions is xuě (blood)[28] - but this is mainly a matter of stipulation, not anatomical insight.[29]
The primary functional entities used by traditional Chinese medicine are qì, xuě, the five zàng organs, the six fǔ organs, and the meridians which extend through the organ systems.[30] These are all theoretically interconnected: each zàng organ is paired with a fǔ organ, which are nourished by the blood and concentrate qi for a particular function, with meridians being extensions of those functional systems throughout the body.
[edit] Qi
TCM distinguishes not only one but several different kinds of qi (氣).[31] In a general sense, qi is something that is defined by five "cardinal functions":[31][32]
- Actuation (推動, tuīdòng) - of all physical processes in the body, especially the circulation of all body fluids such as blood in their vessels. This includes actuation of the functions of the zang-fu organs and meridians.
- Warming (溫煦, pinyin: wēnxù) - the body, especially the limbs.
- Defense (防御, pinyin: fángyù) - against Exogenous Pathogenic Factors
- Containment (固攝, pinyin: gùshè) - of body fluids, i.e. keeping blood, sweat, urine, semen etc. from leakage or excessive emission.
- Transformation (氣化, pinyin: qìhuà) - of food, drink, and breath into qi, xue, and jinye (“fluids”), and/or transformation of all of the latter into each other.
Vacuity of qi will especially be characterized by pale complexion, lassitude of spirit, lack of strength, spontaneous sweating, laziness to speak, non-digestion of food, shortness of breath (especially on exertion), and a pale and enlarged tongue.[13]
Qi is believed to be partially generated from food and drink, and partially from air (by breathing).[33] Another considerable part of it is inherited from the parents and will be consumed in the course of life.[33]
In terms of location, TCM uses special terms for qi running inside of the blood vessels and for qi which is distributed in the skin, muscles, and tissues between those. The former is called yíng-qì (營氣), its function is to complement xuè and its nature has a strong yin aspect (although qi in general is considered to be yang).[34] The latter is called weì-qì (衛氣), its main function is defence and it has pronounced yang nature.[34]
Qi also circulates in the meridians. Just as the qi held by each of the zang-fu organs, this is considered to be part of the ‘’principal‘’ qi (元氣, pinyin: yuán qì) of the body[35] (also called 真氣 pinyin: zhēn qì, ‘’true‘’ qi, or 原氣 pinyin: yuán qì, ‘’original‘’ qi).[36]
[edit] Xue (blood)
In contrast to most of the other functional entities, xuě (血, "blood") is correlated with a physical form - the red liquid running in the blood vessels.[37] Its concept is, nevertheless, defined by its functions: nourishing all parts and tissues of the body, safeguarding an adequate degree of moisture,[38] and sustaining and soothing both consciousness and sleep.[37]
Typical symptoms of a lack of xuě (usually termed "blood vacuity" [血虚, pinyin: xuě xū}) are described as: Pale-white or whithered-yellow complexion, dizziness, flowery vision, palpitations, insomnia, numbness of the extremities; pale tongue; "fine" pulse.[39]
[edit] Jinye (bodily fluids)
Closely related to xuě are the jīnyė (津液, usually translated as ‘’body fluids‘’), and just like xuě they are considered to be yin in nature, and defined first and foremost by the functions of nurturing and moisturizing the different structures of the body.[40] Their other functions are to harmonize yin and yang, and to help with secretion of waste products.[41]
Jīnyė are ultimately extracted from food and drink, and constitute the raw material for the production of xuě; conversely, xuě can also be transformed into jīnyė.[42] Their palpable manifestations are all bodily fluids: tears, sputum, saliva, gastric juice, joint fluid, sweat, urine, etc.[43]
[edit] The zang-fu
The zàng-fǔ (simplified Chinese: 脏腑; traditional Chinese: 臟腑) constitute the centre piece of TCM's systematization of bodily functions. Bearing the names of organs, they are, however, only secondarily tied to (rudimental) anatomical assumptions (the fǔ a little more, the zàng much less).[44] As they are primarily defined by their functions,[45][46] they are not equivalent to the anatomical organs - to highlight this fact, their names are usually capitalized.
The term zàng (脏) refers to the five entities considered to be yin in nature - Heart, Liver, Spleen, Lung, Kidney -, while fǔ (腑) refers to the six yang organs - Small Intestine, Large Intestine, Gallbladder, Urinary Bladder, Stomach and Sānjiaō.[47]
The zàng's essential functions consist in production and storage of qì and blood; in a wider sense they are stipulated to regulate digestion, breathing, water metabolism, the musculoskeletal system, the skin, the sense organs, aging, emotional processes, mental activity etc.[48] The fǔ organs' main purpose is merely to transmit and digest (传化, pinyin: chuán-huà)[49] substances like waste, food, etc.
Since their concept was developed on the basis of Wǔ Xíng philosophy, each zàng is paired with a fǔ, and each zàng-fǔ pair is assigned to one of five elemental qualities (i.e., the Five Elements or Five Phases).[50] These correspondences are stipulated as:
- Fire (火) = Heart (心, pinyin: xīn) and Small Intestine (小肠, pinyin: xiaǒcháng) (and, secondarily, Sānjiaō [三焦, ‘’Triple Burner‘’] and Pericardium [心包, pinyin: xīnbaò])
- Earth (土) = Spleen (脾, pinyin: pí) and Stomach (胃, pinyin: weì)
- Metal (金) = Lung (肺, pinyin: feì) and Large Intestine (大肠, pinyin: dàcháng)
- Water (水) = Kidney (肾, pinyin: shèn) and Bladder (膀胱, pinyin: pǎngguāng)
- Wood (木) = Liver (肝, pinyin: gān) and Gallbladder (胆, pinyin: dān)
The zàng-fǔ are also connected to the twelve standard meridians - each yang meridian is attached to a fǔ organ and five of the yin meridians are attached to a zàng. As there are only five zàng but six yin meridians, the sixth is assigned to the Pericardium, a peculiar entity almost similar to the Heart zàng.[51]
[edit] Meridians
The meridians (经络, pinyin: jīng-luò) are believed to be channels running from the zàng-fǔ in the interior (里, pinyin: lǐ) of the body to the limbs and joints ("the surface" [表, pinyin: biaǒ]), transporting qi and xuĕ (blood).[52][53] TCM identifies 12 "regular" and 8 "extraordinary" meridians;[30] the Chinese terms being 十二经脉 (pinyin: shí-èr jīngmài, lit. "the Twelve Vessels") and 奇经八脉 (pinyin: qí jīng bā mài) respectively.[54] There's also a number of less customary channels branching off from the "regular" meridians.[30]
[edit] Concept of disease
In general, disease is perceived as a disharmony (or imbalance) in the functions or interactions of yin, yang, qi, xuĕ, zàng-fǔ, meridians etc. and/or of the interaction between the human body and the environment.[55]
Therapy is based on which "pattern of disharmony" can be identified.[56][57] Thus, "pattern discrimination" is the most important step in TCM diagnosis.[56][57] It is also known to be the most difficult aspect of practicing TCM.[58] In order to determine which pattern is at hand, practitioners will examine things like the color and shape of the tongue, the relative strength of pulse-points, the smell of the breath, the quality of breathing or the sound of the voice.[59][60] For example, depending on tongue and pulse conditions, a TCM practitioner might diagnose bleeding from the mouth and nose as: "Liver fire rushes upwards and scorches the Lung, injuring the blood vessels and giving rise to reckless pouring of blood from the mouth and nose.".[61] He might then go on to prescribe treatments designed to cool the liver or supplement the lungs.
[edit] Disease entities
In TCM, a disease has two aspects: "bìng" and "zhèng".[62] The former is often translated as "disease entity",[63] "disease category",[64] "illness",[62] or simply "diagnosis".[62] The latter, and more important one, is usually translated as "pattern"[63][65] (or sometimes also as "syndrome"[62]). For example, the disease entity of a common cold might present with a pattern of wind-cold in one patient, and with the pattern of wind-heat in another.[66]
From a scientific point of view, most of the disease entitites (病, pinyin: bìng) listed by TCM constitute mere symptoms.[63] Examples include headache, cough, abdominal pain, constipation etc.[67]
Since therapy will not be chosen according to the disease entity but according to the pattern, two patients with the same disease entity but different patterns will receive different therapy. Vice versa, patients with similar patterns might receive similar therapy even if their disease entities are different. This is called 异病同治,同病异治 (pinyin: yì bìng tóng zhì, tóng bìng yì zhì,[57] "different diseases, same treatment; same disease, different treatments").
[edit] Patterns
In TCM, "pattern" (证, pinyin: zhèng) refers to a "pattern of disharmony" or "functional disturbance" within the functional entities the TCM model of the body is composed of.[68] There are disharmony patterns of qi, xuě, the body fluids, the zàng-fǔ, and the meridians.[69] They are ultimately defined by their symptoms and "signs" (i.e., for example, pulse and tongue findings).[70]
In clinical practise, the identified pattern usually involves a combination of affected entities[71] (compare with typical examples of patterns). The concrete pattern identified should account for all the symptoms a patient has.[72]
[edit] The Six Excesses
The Six Excesses (六淫, pinyin: liù yín,[73] sometimes also translated as "Pathogenic Factors",[74] or "Six Pernicious Influences";[75] with the alternative term of 六邪, pinyin: liù xié, - "Six Evils" or "Six Devils"[76]) are allegorical terms used to describe disharmony patterns displaying certain typical symptoms.[77] These symptoms resemble the effects of six climatic factors.[75] In the allegory, these symptoms can occur because one or more of those climatic factors (called 六气, pinyin: liù qì, "the six qi"[78]) were able to invade the body surface and to proceed to the interior.[79] This is sometimes used to draw causal relationships (i.e., prior exposure to wind/cold/etc. is identified as the cause of a disease),[80] while other authors explicitly deny a direct cause-effect relationship between weather conditions and disease,[81][82] pointing out that the Six Excesses are primarily descriptions of a certain combination of symptoms[83] translated into a pattern of disharmony.[75]
It is undisputed, though, that the Six Excesses can manifest inside the body without an external cause.[79][84] In this case, they might be denoted "internal", e.g., "internal wind"[84] or "internal fire (or heat)".[85]
The Six Excesses and their characteristic clinical signs are:
- Wind (风, pinyin: fēng): rapid onset of symptoms, wandering location of symptoms, itching, nasal congestion, "floating" pulse;[86] tremor, paralysis, convulsion.[79]
- Cold (寒, pinyin: hàn): cold sensations, aversion to cold, relief of symptoms by warmth, watery/clear excreta, severe pain, abdominal pain, contracture/hypertonicity of muscles, (slimy) white tongue fur, "deep"/"hidden" or "string-like" pulse,[87] or slow pulse.[88]
- Fire/Heat (火, pinyin: huǒ): aversion to heat, high fever, thirst, concentrated urine, red face, red tongue, yellow tongue fur, rapid pulse.[89] (Fire and heat are basically seen to be the same)[90]
- Dampness (湿, pinyin: shī): sensation of heaviness, sensation of fullness, symptoms of Spleen dysfunction, greasy tongue fur, "slippery" pulse.[88]
- Dryness (燥, pinyin: zaò): dry cough, dry mouth, dry throat, dry lips, nosebleeds, dry skin, dry stools.[91]
- Summerheat (署, pinyin: shǔ): either heat or mixed damp-heat symptoms.[92]
Six-Excesses-patterns can consist of only one or a combination of Excesses (e.g., wind-cold, wind-damp-heat).[86] They can also transform from one into another.[86]
[edit] Typical examples of patterns
For each of the functional entities (qi, xuĕ, zàng-fǔ, meridians etc.), typical disharmony patterns are recognized; for example: qi vacuity and qi stagnation in the case of qi;[93] blood vacuity, blood stasis, and blood heat in the case of xuĕ;[94] Spleen qi vacuity, Spleen yang vacuity, Spleen qi vacuity with down-bearing qi, Spleen qi vacuity with lack of blood containment, cold-damp invasion of the Spleen, damp-heat invasion of Spleen and Stomach in case of the Spleen zàng;[95] wind/cold/damp invasion in the case of the meridians.[96]
TCM gives detailed prescriptions of these patterns regarding their typical symptoms, mostly including characteristic tongue and/or pulse findings.[97][98] For example:
- "Upflaming Liver fire" (肝火上炎, pinyin: gānhuǒ shàng yán): Headache, red face, reddened eyes, dry mouth, nosebleeds, constipation, dry or hard stools, profuse menstruation, sudden tinnitus or deafness, vomiting of sour or bitter fluids, expectoration of blood, irascibility, impatience; red tongue with dry yellow fur; slippery and string-like pulse.[99]
[edit] Basic principles of pattern discrimination
The process of determining which actual pattern is on hand is called 辩证 (pinyin: biàn zhèng, usually translated as "pattern diagnosis",[100] "pattern identification"[101] or "pattern discrimination"[65]). Generally, the first and most important step in pattern diagnosis is an evaluation of the present signs and symptoms on the basis of the "Eight Principles" (八纲, pinyin: bā gāng).[101][102] These eight principles refer to four pairs of fundamental qualities of a disease: exterior/interior, heat/cold, vacuity/repletion, and yin/yang.[101] Out of these, heat/cold and vacuity/repletion have the biggest clinical importance.[101] The yin/yang quality, on the other side, has the smallest importance and is somewhat seen aside from the other three pairs, since it merely presents a general and vague conclusion regarding what other qualities are found.[101] In detail, the Eight Principles refer to the following:
- Exterior (表, pinyin: biaǒ) refers to a disease manifesting in the superficial layers of the body - skin, hair, flesh, and meridians.[103] It is characterized by aversion to cold and/or wind, headache, muscle ache, mild fever, a "floating" pulse, and a normal tongue appearance.[103]
- Interior (里, pinyin: lǐ)refers to disease manifestation in the zàng-fǔ, or (in a wider sense) to any disease that can not be counted as exterior.[104] There are no generalized characteristic symptoms of interior patterns, since they'll be determined by the affected zàng or fǔ entity.[105]
- Cold (寒, pinyin: hàn) is generally characterized by aversion to cold, absence of thirst, and a white tongue fur.[106] More detailed characterization depends on whether cold is coupled with vacuity or repletion.[106]
- Heat (热, pinyin: rè) is characterized by absence of aversion to cold, a red and painful throat, a dry tongue fur and a rapid and floating pulse, if it falls together with an exterior pattern.[107] In all other cases, symptoms depend on whether heat is coupled with vacuity or repletion.[108]
- Vacuity (虚, pinyin: xū) can be further differentiated into vacuity of qi, xuě, yin and yang, with all their respective characteristic symptoms.[109] Yin vacuity can also be termed "vacuity-heat", while yang vacuity is equivalent to "vacuity-cold".[110]
- Repletion (实, pinyin: shí) generally refers to any disease that can't be identified as a vacuity pattern, and usually indicates the presence of one of the Six Excesses,[111] or a pattern of stagnation (of qi, xuě, etc.).[112] In a concurrent exterior pattern, repletion is characterized by the absence of sweating.[107] The signs and symptoms of repletion-cold patterns are equivalent to cold excess patterns, and repletion-heat is similar to heat excess patterns.[113]
- Yin and yang are universal aspects all things can be classified under, this includes diseases in general as well as the Eight Principles' first three couples.[114] For example, cold is identified to be a yin aspect, while heat is attributed to yang.[114] Since descriptions of patterns in terms of yin and yang lack complexity and clinical practicality, though, patterns are usually not labelled this way anymore.[114] Exceptions are vacuity-cold and repletion-heat patterns, who are sometimes referred to as "yin patterns" and "yang patterns" respectively.[114]
After the fundamental nature of a disease in terms of the Eight Principles is determined, the investigation focuses on more specific aspects.[101] By evaluating the present signs and symptoms against the background of typical disharmony patterns of the various entities, evidence is collected whether or how specific entities are affected.[115] This evaluation can be done
- in respect of the meridians (经络辩证, pinyin: jīng-luò biàn zhèng)[71]
- in respect of qi (气血辩证, pinyin: qì xuě biàn zhèng)[65]
- in respect of xuě (气血辩证, pinyin: qì xuě biàn zhèng)[65]
- in respect of the body fluids (津液辩证, pinyin: jīn-yė biàn zhèng)[65]
- in respect of the zàng-fǔ (脏腑辩证, pinyin: zàng-fǔ biàn zhèng)[65] - very similar to this, though less specific, is disharmony pattern description in terms of the Five Elements [五行辩证, pinyin: wǔ xíng biàn zhèng][116])
There are also three special pattern diagnosis systems used in case of febrile and infectious diseases only ("Six Channel system" or "six division pattern" [六经辩证, pinyin: liù jīng biàn zhèng]; "Wei Qi Ying Xue system" or "four division pattern" [卫气营血辩证, pinyin: weì qì yíng xuě biàn zhèng]; "San Jiao system" or "three burners pattern" [三角辩证, pinyin: sānjiaō biàn zhèng]).[69][117]
[edit] Considerations of disease causes
Although TCM and its concept of disease do not strongly differentiate between cause and effect,[118] pattern discrimination can include considerations regarding the disease cause; this is called 病因辩证 (pinyin: bìngyīn biàn zhèng, "disease-cause pattern discrimination").[71]
There are three fundamental categories of disease causes (三因, pinyin: sān yīn) recognized:[55]
- external causes: these include the Six Excesses and "Pestilential Qi".[55]
- internal causes: the "Seven Affects" (七情, pinyin: qì qíng,[55] sometimes also translated as "Seven Emotions"[119]) - joy, anger, pensiveness, sorrow, fear, fright and grief.[119] These are believed to be able to cause damage to the functions of the zàng-fú, especially of the Liver.[120]
- non-external-non-internal causes: dietary irregularities (especially: too much raw, cold, spicy, fatty or sweet food; voracious eating; too much alcohol),[121] fatigue, sexual intemperance, trauma, and parasites (虫, pinyin: chóng).[55]
[edit] Medicines
-
- "The method of appropriately using herbs in accordance with the symptom and sign presentation of the patient entails determining substances with the correct qi, taste, yin and yang, and thick and thin properties as well as the pathogenic factor involved and the meridian it has entered." - Zhang Jiegu



Traditional Chinese medicines are made from plants and herbs, and occasionally from organ meats or other substances. Medicinals are typically constructed from a number of materials designed - according to its theory - to stimulate certain organ systems or to balance out the undesired aspects of other materials used. These are often provided in dried form to be steeped into a tea, though practitioners may suggest them as dietary changes instead - adding certain organ meats or herbs to meals, for instance - or they may be powdered and used in pill form. There are roughly 13,000 medicinals used in China and over 100,000 medicinal recipes recorded in the ancient literature.[122] Some conceptions of the theory believe that toxicity is needed to fight pathogens in the body, similar to homeopathy,[123] so chemicals considered to be toxic are used in some preparations. Further, ingredients may have different names in different locales or in historical texts, and different preparations may have similar names for the same reason, which creates inconsistencies and confusion in the creation of medicinals.[124] resulting in poisoning.[125][126][127]
Plant elements and extracts are by far the most common elements used in medicines.[128] In the classic Handbook of Traditional Drugs from 1941, 517 drugs were listed - out of these, 45 were animal parts, and 30 were minerals.[128] Snake oil, which is used traditionally for joint pain as a liniment,[129] is the most widely known Chinese medicine in the west, due to extensive marketing in the west in the late 1800s and early 1900s, and wild claims of its efficacy to treat many maladies; however, there is no clinical evidence that it is effective.[129][130]
Certain ingredients used traditionally can be dangerous, such as secretions from the Asiatic toad,[131] powdered centipede,[132] the Chinese beetle (Mylabris phalerata, Ban mao),[133] and certain fungi.[134]
The animal parts can be considered rather strange such as cows' gallstones,[135] and can include the parts of endangered species, including tiger penis[136][137] and rhinoceros horn.[138] The black market in rhinoceros horn decimated the world's rhino population by more than 90 percent over the past 40 years.[139] Concerns have also arisen over the use of turtle plastron[140] and seahorses.[141] In general, Chinese traditional medicine emphasizes the penis of animals as therapeutic.[136] Traditional Chinese Medicine also includes some human parts: the classic Materia medica (Bencao Gangmu) describes the use of 35 human body parts and excreta in medicines, including bones, fingernail, hairs, dandruff, earwax, impurities on the teeth, feces, urine, sweat, organs, but most are no longer in use.[142][143][144]
Ginseng is the most broadly used substance for the most broad set of alleged cures. Powdered pre-calcified antler, horns, teeth, and bones are second in importance to ginseng, with claims ranging from curing cancer to improving immune system function to curing impotence.
| Aconite root | Aconite root (wolfsbane) is a root commonly used in TCM.[145] Aconite root contains neurotoxin aconitine, which is a potent toxin.[146] There is no antidote. |
| Arsenic (Realgar) | Arsenic sulfide (Realgar, xiong huang) is a toxic mineral used in TCM under the belief that it kills intestinal parasites, treats sore throats, treat swellings, abscesses, itching, and rashes.[147] It is most commonly sold as a powder and given as a pill or capsule, although it is also incorporated into a mixture with other TCM medicinal ingredients.[147] |
| Actinolitum | Actinolitum is not a commonly used substance, but has been used to treat impotence. It is toxic in its fibrous form.[148] |
| Beetle | Chinese beetle (Mylabris phalerata, Ban mao) is believed under TCM to treat skin lesions, because it causes them.[149][150] It contains the toxic chemical cantharidin.[133] |
| Camellia | Camellia tea from India, Sri Lanka, Java, Japan is used in TCM for aches and pains, digestion, depression, detoxification, as an energizer and, to prolong life.[151] |
| Cayenne | Cayanneis believed under TCM to be a prophylactic medicine.[152] |
| Centipede | Powdered centipede (wu gong) is believed under TCM to treat lockjaw, seizures, convulsions, skin lesions, and pain.[132] It is toxic.[132] |
| Chinese cucumber | Chinese cucumber (Trichosanthes kirilowi) is believed to treat tumors, reduce fevers, swelling and coughing, abscesses, amenorrhea, jaundice, and polyuria. Extracts are extremely toxic. Side effects include hormone changes, allergic reaction, fluid in the lungs or brain, bleeding in the brain, heart damage, seizures, and fever.[153] |
| Chrysanthemum flowers | Chrysanthemum flowers (Ju Hua) are used in TCM under a belief that it treats headaches, fever, dizziness and dry eyes. It is also popular for use in teas as a beverage.[154] |
| Cocklebur fruit | Cocklebur fruit (Xanthium, cang er zi) is one of the most important herbs in TCM, which believes it can be used to treat sinus congestion, chronic nasal obstructions and discharges, and respiratory allergies.[155] Xanthium is toxic and causes vomiting, diarrhea and abdominal pain.[156] |
| Cow dipper | Cow dipper (sheng ban xia, Pinellia ternata) is believed under TCM to be the strongest of all TCM herbs for removing phlegm.[157] Cow dipper is highly toxic to humans.[158] Traditional Chinese medicine advocates believe toxicity can be reduced in their method of preparation.[157] |
| Croton seed | Croton seed (Croton tiglium)is believed under TCM to treat gastrointestinal disorders, convulsions, and skin lesions. It is often used with rhubarb, dried ginger and apricot seed.[159] Croton contains cancer causing chemicals.[160] |
| Deer penis | Deer penis is commonly sold in Chinese pharmacies as an effective remedy for athletic injuries, to enhance male virility, and to be an aphrodisiac.[161][162][citation needed] China banned deer penis during the 2008 Summer Olympics. |
| Ginger | Ginger root Zingiber officinale) has been used in China for over 2,000 years under a belief that it aids digestion and treats upset stomach, diarrhea, and nausea. TCM also teaches that it helps treat arthritis, colic, diarrhea, and heart conditions. Traditional Chinese medicine believes that it treats the common cold, flu-like symptoms, headaches, and menstrual cramps. Today, health care professionals commonly recommend to help prevent or treat nausea and vomiting associated with motion sickness, pregnancy, and cancer chemotherapy. It is also used as a digestive aid for mild stomach upset, as support in inflammatory conditions such as arthritis, and may even be used in heart disease or cancer.[163] |
| Ginkgo biloba | seeds are crushed and believed under TCM to treat asthma.[164] Ginkgo has been used in TCM for nearly 5,000 years.[165] Further studies to establish the efficacy both as used under TCM beliefs and for proposed uses as an evidence based medicine are required.[165] |
| Ginseng | Ginseng root is the most widely sold traditional Chinese medicine. The name "ginseng" is used to refer to both American (Panax quinquefolius) and Asian or Korean ginseng (Panax ginseng), which belong to the species Panax and have a similar chemical makeup. Siberian ginseng or Eleuthero (Eleutherococcus senticosus) is another type of plant. Asian ginseng has a light tan, gnarled root that often looks like a human body with stringy shoots for arms and legs. In ancient times, herbalists thought that because of the way ginseng looks it could treat many different kinds of syndromes, from fatigue and stress to asthma and cancer. In traditional Chinese medicine, ginseng was often combined with other herbs and used often to bring longevity, strength, and mental alacrity to its users. Asian ginseng is believed to enhance the immune system in preventing and treating infection and disease. Several clinical studies report that Asian ginseng can improve immune function. Studies have found that ginseng seems to increase the number of immune cells in the blood, and improve the immune system's response to a flu vaccine. In one study, 227 participants received either ginseng or placebo for 12 weeks, with a flu shot administered after 4 weeks. The number of colds and flu were two-thirds lower in the group that took ginseng.[166]| |
| Goji berry | Marketing literature for goji berry (wolfberry) products including several "goji juices" suggest that wolfberry polysaccharides have extensive biological effects and health benefits. |A May 2008 clinical study published by the peer-reviewed Journal of Alternative and Complementary Medicine indicated that parametric data, including body weight, did not show significant differences between subjects receiving Lycium barbarum berry juice and subjects receiving the placebo; the study concluded that subjective measures of health were improved and suggested further research in humans was necessary.[167] This study, however, was subject to a variety of criticisms concerning its experimental design and interpretations.[168] |
| Hornets nest | Hornets nest (lu feng fang) is used under a belief that it can treat skin disorders and ringworm.[169] It may be toxic.[133] |
| Horny goat weed | Horny goat weed (Epimedium spp., Yin Yang Huo, 淫羊藿) is believed to be an aphrodisiac.[170] Exploitation of wild populations is having potentially serious consequences for the long-term survival of several species.[171] |
| Lead (Galena) | Lead oxide (Galena, mi tuo seng) is believed under TCM to treat ringworm, skin disorders, and ulcers. It is crushed and taken orally or used on the skin. Lead is toxic to humans.[172] |
| Mercury (Cinnabar) | Despite its toxicity, sulfide of mercury (cinnabar) has historically been used in Chinese medicine, where it is called zhūshā (朱砂), and was highly valued in Chinese Alchemy. It was also referred to as dān (丹), meaning all of Chinese alchemy, cinnabar, and the "elixir of immortality". Cinnabar (HgS, sulfide of mercury) has been used in Traditional Chinese medicine as a sedative for more than 2000 years, and has been shown to have sedative and toxic effects in mice.[173] |
| Rhinoceros horn | Rhinoceros horn is used as an antifever agent, because it is believed to "cool the blood".[138] The black market in rhinoceros horn decimated the world's rhino population by more than 90 percent over the past 40 years.[139] |
| Leech | Leech (shui zhi) is believed under TCM to treat amenorrhea, abdominal and chest pain, and constipation.[174] It is toxic and so is believed under TCM to treat toxics.[149][174] |
| Rhubarb | Rhubarb (大黄) is a large root and was once one of the first herbs that was imported from China.[175] |
| Scorpion | Sorpions (quan xie) are ground into a powder and mixed with water.[176] Scorpions are poisonous. Powdered scorpion is toxic, so is believed to be usable to treat other toxins.[176] |
| Seahorse | Seahorse fish is a fundamental ingredient in therapies for a variety of disorders, including asthma, arteriosclerosis, incontinence, impotence, thyroid disorders, skin ailments, broken bones, heart disease, as well as to facilitate childbirth and even as an aphrodisiac.[141] |
| Thunder Vine | Thunder Vine (Lei Gong Teng, Radix tripterygii wilfordii, or lei gong teng) use is on the rise in TCM because of a belief under TCM that it treats arthritis, relieves pain and reduces joint swelling.[177] It is an extremely toxic.[177] Within two to three hours after ingestion, a patient may begin to have gastrointestinal problems, headache, dizziness, severe vomiting (sometimes with blood), chills, high fever, and irregular heart beat. Damage to the central nervous system follows, as well as internal bleeding of the (real) organs, then their necrosis.[177] |
| Shark fin | Shark fin soup is traditionally regarded as beneficial for health in East Asia.[178] |
| Strychnine tree seeds | Strychnine tree seeds (Strychnos nux-vomica, Ma Qian Zi) are marketed and sold with a claim to treat diseases of the respiratory tract, anemia, and geriatric complaints. It contains toxic strychnine, so can also be used as a poison for rodents.[179] Dan Besky writes in his Materia Medica that "due to the small difference between the therapeutic and toxic doses, use of strychni semen (ma quian zi) bears a high risk of inducing severe poisoning and for this reason should be regarded as an obsolete drug".[180] |
| Sweet wormwood | Sweet wormwood (Artemisia annua, Qing Hao) is believed under TCM to treat fever, headache, dizziness, stopping bleeding, and alternating fever and chills.[181] It had fallen out of common use under TCM until it was rediscovered in 1970's when the Chinese Handbook of Prescriptions for Emergency Treatments (340 AD) was found. This pharmacopeia contained recipes for a tea from dried leaves, prescribed for fevers (not specifically malaria). The plant extracts in TCM have the antimalarial artemisinin.[182]| |
| Supernatural mushroom | The supernatural mushroom (lingzhi mushroom, Chinese “linh chi” = “supernatural mushroom”, "reishi mushroom" in Japan) encompasses several fungal species of the genus Ganoderma, and most commonly refers to the closely related species, Ganoderma lucidum and Ganoderma tsugae. G. lucidum enjoys special veneration in East Asia, where it has been used as a medicinal mushroom in traditional Chinese medicine for more than 2,000 years,[183] making it one of the oldest mushrooms known to have been used medicinally.| |
| Tiger penis | Popular "medicinal" tiger parts from poached animals include tiger penis, believed to improve virility, and tiger eyes.[136][184] Laws protecting even critically endangered species such as the Sumatran Tiger fail to stop the display and sale of these items in open markets.[137] |
| Turtle shell | |
| Willow bark | Salix genus plants were used since the time of Hippocrates (400 BC) when patients were advised to chew on the bark to reduce fever and inflammation. Willow bark has been used throughout the centuries in China and Europe to the present for the treatment of pain (particularly low back pain and osteoarthritis), headache, and inflammatory conditions such as bursitis and tendinitis. The bark of white willow contains salicin, which is a chemical similar to aspirin (acetylsalicylic acid). It is thought to be responsible for the pain-relieving and anti-inflammatory effects of the herb. In the 1829, salicin was used to develop aspirin. White willow appears to be slower than aspirin to bring pain relief, but its effects may last longer.[185] |
[edit] Efficacy
Regarding Traditional Chinese herbal therapy, only few trials of adequate methodology exist and its effectiveness therefore remains poorly documented.[186]
[edit] Pills and powders
The TCM industry traditionally supplied medicines as powders to be measured and/or compounded by individual practitioners. More recently, soluble granules and tablets have become available with specific dosage levels. Modern formulations in pills and sachets used 675 plant and fungi ingredients and about 25 from non-plant sources such as snakes, geckos, toads, frogs, bees, and earthworms.[citation needed]
[edit] Chinese alchemy (Pao zhi)
Chinese alchemy (Pao zhi, Pao chi) refers to the alchemy of processing medicines in TCM, such as honey or wine frying and roasting with toxic metals such as mercury, lead, and arsenic.[187][188]
[edit] Ecological impacts of use of medicines
Animal products are used in certain Chinese preparations, which may disturb conservationists, vegans and vegetarians. If informed of such restrictions, practitioners can often use alternative substances.
The practice of using endangered species is controversial within TCM. Modern Materia Medicas such as Bensky, Clavey and Stoger's comprehensive Chinese herbal text discuss substances derived from endangered species in an appendix, emphasizing alternatives.[189]
Poachers hunt restricted animals to supply the black market for such products.[190][191]
The animal rights movement claims that traditional Chinese medicinal solutions still use bear bile (xíong dǎn). In 1988, the Chinese Ministry of Health started controlling bile production, which previously used bears killed before winter. Now bears are fitted with a sort of permanent catheter, which was more profitable than killing the bears.[192] The treatment itself and especially the extraction of the bile is very painful, and damages their stomach and intestines, often resulting in their eventual death. Increased international attention has mostly stopped the use of bile outside of China; gallbladders from butchered cattle (niú dǎn / 牛膽 / 牛胆) are recommended as a substitute for this ingredient.
Medicinal use is impacting seahorse populations.
Ecological effects are greater than just on the species used in TCM. The worldwide shark population has been devastated to a small fraction of its original population by a growing demand for shark fin soup. Sharks fins are cut off and the live shark which is then dumped back in the ocean to sink and slowly die. Once considered only for rare occasions, with a growing Asian middle class, there is an accompanying demand for shark fin. Sharks take many years to mature to give birth. The problem does not only affect sharks. Since sharks are the top predator in the food chain, the impact on shark populations threatens to throw the entire marine ecosystem out of balance, with an unpredictable outcome.[193]
[edit] Techniques
[edit] Acupuncture, moxibustion, and auriculotherapy
Acupuncture is an alternative medicine that treats patients by insertion and manipulation of needles in the body. Its proponents variously claim that it relieves pain, treats infertility, treats disease, prevents disease, promotes general health, or can be used for therapeutic purposes.[194] Acupuncture typically incorporates traditional Chinese medicine (TCM) as an integral part of its practice and theory. The term “acupuncture” is sometimes used to refer to insertion of needles at points other than traditional ones, or to applying an electric current to needles in acupuncture points.[195][196] Acupuncture dates back to prehistoric times, with written records from the second century BCE. Different variations of acupuncture are practiced and taught throughout the world.
Acupuncture is often accompanied by moxibustion, which involves burning mugwort on or near the skin at an acupuncture point.[197] There are three methods of moxibustion: Direct scarring, direct non-scarring, and indirect moxibustion. Direct scarring moxibustion places a small cone of mugwort on the skin at an acupuncture point and burns it until the skin blisters, which then scars after it heals.[197] Direct non-scarring moxibustion removes the burning mugwort before the skin burns enough to scar, unless the burning mugwort is left on the skin too long.[197] Indirect moxibustion holds a cigar made of mugwort near the acupuncture point to heat the skin, or holds it on an acupuncture needle inserted in the skin to heat the needle.[197] The Chinese character for acupuncture means "acupuncture-moxibustion".
Auriculotherapy (耳灼疗法/耳燭療法) applies acupuncture or moxibustion to the ear. It is believed that a part of the ear (the auricle) is a microsystem with the entire body represented on it.
The effectiveness of acupuncture beyond the placebo effect is not well established.[198] A systematic review found that acupuncture is no more effective than a nonpenetrating sham treatment for treating post operative nausea.[199][200] A 2008 meta analysis pooling studies without placebos with those that had them concluded that combining acupuncture with conventional infertility treatments such as IVF improves the success rates of such medical interventions, but did not conclude that acupuncture was more effective than a sham treatment.[201] There is conflicting evidence that it can treat chronic low back pain,[202][203] and moderate evidence of efficacy for neck pain[204][205] and headache.[206] For most other conditions[207] reviewers have found either a lack of efficacy (e.g., help in quitting smoking[208]) or have concluded that there is insufficient evidence to determine if acupuncture is effective (e.g., treating shoulder pain[209]). While little is known about the mechanisms by which acupuncture may act, a review published in an alternative medicine journal of neuroimaging research suggests that specific acupuncture points have distinct effects on cerebral activity in specific areas that are not otherwise predictable anatomically.[210] The website Quackwatch mentions that TCM has been the subject of criticism as having unproven efficacy and an unsound scientific basis.[211]
The evidence for acupuncture's effectiveness for anything but the relief of some types of pain and nausea has not been established.[212][213][214] Systematic reviews have concluded that acupuncture is no more effective than nonpenetrating stimulation of one point to reduce some types of nausea.[199] Evidence for the treatment of other conditions is equivocal.[198] Although evidence exists for a very small and short-lived effect on some types of pain, several review articles discussing the effectiveness of acupuncture have concluded it is possible to explain as a placebo effect.[212][215] Publication bias is a significant concern when evaluating the literature. Reports from the US National Center for Complementary and Alternative Medicine In America (NCCAM), the American Medical Association (AMA) and various US government reports have studied and commented on the efficacy of acupuncture. There is general agreement that acupuncture is safe when administered by well-trained practitioners using sterile needles.[216][217][218] The World Health Organization (WHO) has compiled a list of disorders for which acupuncture might have an effect; adverse reactions to chemotherapy and radiation, induction of labor, sciatica, dysmenorrhea, depression, hypertension, rheumatoid arthritis, and low back pain.[219]
[edit] Cupping
Cupping (拔罐) is a type of Chinese massage, consisting of placing several glass "cups" (open spheres) on the body. A match is lit and placed inside the cup and then removed before placing the cup against the skin. As the air in the cup is heated, it expands, and after placing in the skin, cools, creating lower pressure inside the cup that allows the cup to stick to the skin via suction. When combined with massage oil, the cups can be slid around the back, offering "reverse-pressure massage".===
[edit] Die-da or Tieh Ta
Die-da or Tieh Ta (跌打) is usually practiced by martial artists who know aspects of Chinese medicine that apply to the treatment of trauma and injuries such as bone fractures, sprains, and bruises. Some of these specialists may also use or recommend other disciplines of Chinese medical therapies (or Western medicine in modern times) if serious injury is involved. Such practice of bone-setting (整骨) is not common in the West.
[edit] Gua Sha
Gua Sha (“to lift up for cholera”, or “to scrape for cholera”) is abrading the skin with pieces of smooth jade, bone, animal tusks or horns or smooth stones; until red spots then bruising cover the area to which it is done. It is believed that this treatment is for almost any ailment including cholera. The red spots and bruising take 3 to 10 days to heal. It is believed that most people can tolerate the pain of treatment, but there is often some soreness in the area that has been treated.[220][221][222][223]
[edit] Physical Qigong exercises
Physical Qigong exercises such as Tai chi chuan (Taijiquan 太极拳/太極拳), Standing Meditation (站樁功), Yoga, Brocade BaDuanJin exercises (八段锦/八段錦) and other Chinese martial arts.
[edit] Breathing and meditation exercise
Qigong (气功/氣功) and related breathing and meditation exercise.
[edit] Massage
Tui na (推拿) massage: a form of massage akin to acupressure (from which shiatsu evolved). Oriental massage is typically administered with the patient fully clothed, without the application of grease or oils. Choreography often involves thumb presses, rubbing, percussion, and stretches.
[edit] Fengshui aesthetics and Chinese astrology
TCM doctors may also incorporate beliefs about the alignment of buildings with astrological bodies such as the sun (Fengshui aesthetics, 风水/風水), or astrological beliefs about the year, month, date, and hour of birth. Astrological considerations such planting a plant on the solstice or in the correct location (Di Dao Yao Cai) are believed to be important as to a medicine's effectiveness or toxicity.[224][225]
The Four Pillars of Destiny (Bazi, 八字) are the four components believed under TCM to create a person's destiny or fate. The four components within the moment of birth are the year, the month, the day, and the hour, and are used alongside fortune telling practices such as Zǐ wēi dòu shù within the realm of Chinese Astrology as part of diagnosing patients or considerations about medicines.[24][224][226][227][228]
[edit] History


The practice of acupuncture probably dates back to the stone age, as suggested by findings of ancient stone needles.[229] Also, hieroglyphs and pictographs documenting acupuncture and moxibustion have been found which are dating back to the Shang Dynasty (1600-1100 BC).[230]
When acupuncture (and herbal medicine) became integrated into an embracing medical theory system is difficult to judge.[citation needed] TCM theory is, however, inextricably intertwined with the principles of Yinyangism,[231] which was represented for the first time by Zōu Yǎn (340 - 260 BC)).[4]
The earliest and most fundamental composition identified in TCM is the Huăngdì Neìjīng[232] (黄帝内经, Yellow Emperor's Inner Canon), probably dating back to the second century BC.[233] According to legend, it was composed by the mythical Yellow Emperor (said to have lived 2697 - 2597 BC)[234] as a result of a dialogue with his ministers.[232]
Mythical origin was also claimed regarding the Shénnóng Běn Cǎo Jīng (神农本草经, Shennong's Materia Medica) - it traditionally was attributed to the legendary emperor Shénnóng (神农, lit. "Divine Farmer"), said to have lived around 2800 BC.[235] The original text has been lost, however, there are extant translations.[236] The true date of origin is believed to fall into the late Western Han dynasty[235] (i.e., the first century BC).
[edit] Zhang Zhongjing, "Saint of Medicine"
"In terms of the high level, medicine is for curing nobles of their diseases; in terms of the lower level, it is used to save the poor from disaster; in terms of the middle level, it is used to keep us in good health" - "Saint in Medicine".[237]
Zhang Zhongjing born in the later Eastern Han Dynasty, when a pestilence devastated the lives of two thirds of the people in just one decade, and febrile diseases caused by cold accounted for 70% of this. Zhang Zhongjing wrote the Treatise on Febrile Diseases Caused by Cold and Miscellaneous Diseases, which established the principle of treatment according to syndrome differentiation, had numerous new and old medicinal recipes, and established the six channels basis of treatment.[237]
[edit] Hua Tuo, “Originator of Surgery”
Hua Tuo (145 - 208A.D.), a physician of the Eastern Han Dynasty, lived in the same period as physician Zhang Zhongjing. The original of his book Zhongzang Classic is lost, but partially reconstructed by people in the Song Dynasty. It contains mouth-to-mouth resuscitation, a general anesthetic for surgery made with alcohol and mafeisan, and the “Five Mimic-Animal Exercise”, and original surgical procedures using a cutting bone. Mafeisan, is a powder most likely made of Stramonium flowers, which was believed to make patients numb after being washed down with alcohol, and then surgery could be carried out. He traveled to numerous places, collecting formulas, medicines, and knowledge from the local people.[238]
[edit] Sun Simiao, “King of Medicine”[239]
"A Great Physician should not pay attention to status, wealth or age; neither should he question whether the particular person is attractive or unattractive, whether he is an enemy or friend, whether he is a Chinese or a foreigner, or finally, whether he is uneducated or educated. He should meet everyone on equal grounds. He should always act as if he were thinking of his close relatives."[240]
Sun Simiao (581—682 A.D.) is called and “the father of Chinese medical theory”.[239] He wrote the earliest Chinese encyclopedia of medicine, the highly influential Essential Recipes worth a Thousand Gold (Qianjin Yaofang) and A Supplement to Recipes worth a Thousand Gold (Qianjin Yifang).[239] The two books summarized pre Tang Dynasty medicine.[239] The former listed about 5300 recipes for medicines, and the latter 2000. He put forth the “Thirteen measures to keep health”, which claimed that actions like touching hair, rolling eyes, walking, and shaking heads improved health.[239] He also claimed that medicine should be ethical, and wrote "On the Absolute Sincerity of Great Physicians" called "the Chinese Hippocratic Oath," and which is still required reading for Chinese physicians.[239][240] It is said that Sun lived 141 years.[citation needed]
[edit] Tao Hongjing
Tao Hongjing depicted five shen herbs (renshen, danshen, xuanshen, kushen, and shashen; ginseng, salvia, scrophularia, sophora, and adenophora, respectively).
[edit] Zhang Jiegu (Zhang Yuansu)
"The method of appropriately using herbs in accordance with the symptom and sign presentation of the patient entails determining substances with the correct qi, taste, yin and yang, and thick and thin properties as well as the pathogenic factor involved and the meridian it has entered." - Zhang Jiegu
Zhang Jiegu (Zhang Yuansu; ca. 1151-1234) integrated medicinal materials into the five element framework (Wuxing) with both the five shen herbs (spirit herbs) framework and qi meridians. He helped to more clearly define the association of the "tastes" of medicinals and their believed effect on the different organ systems. Zhang asserted that herbs entered into and influenced the meridians. The culmination of Zhang's work was the Bag of Pearls (Zhenzhu Nang, zhenzhu = pearl; nan = bag).
[edit] Li Shizhen
Li Shizhen (1518-1593 AD) wrote the Compendium of Materia Medica (Bencao Gangmu), one of the most frequently mentioned books in the Chinese herbal tradition, rivaled only by the Shanghan Lun.[241][242] It was published in 1596 A.D., three years after his death.[241] It describes the use of human body parts and excreta in medicines, such as the penis, semen, menstrual blood, pubic hair, urine, placenta, fingernails, bones, dandruff, earwax, impurities on the teeth, feces, urine, sweat, and organs.[142][143][144][241]
| Han Dynasty (206 BC–AD 220) to Three Kingdoms Period (220 - 280 AD) |
|
| Jin Dynasty (265 - 420) |
|
| Tang Dynasty (618 - 907) |
|
| Song Dynasty (960 – 1279): |
|
| Yuan Dynasty (1271–1368) |
|
| Ming Dynasty (1368–1644, considered the golden age of acupuncture and moxibustion, spawning many famous doctors and books)[citation needed] |
|
| Qing Dynasty (1644–1912): |
|
| This article cites its sources but does not provide page references. You can help to improve it by introducing citations that are more precise. |
[edit] New age
TCM was more broadly introduced to an America with recent the rise of the New age fascination with magical thinking regarding the mystical concepts of TCM, was introduced to an America infatuated with New Age magical thinking.[245][246]
[edit] See also
- Alternative medicine
- American Journal of Chinese Medicine (journal)
- Ayurveda
- Chinese classic herbal formula
- Chinese food therapy
- Chinese herbology
- Chinese patent medicine
- List of branches of alternative medicine
- List of topics characterized as pseudoscience
- Medicinal mushrooms
- Pharmacognosy
- Public health in the People's Republic of China
- Traditional Korean medicine
- Traditional Mongolian medicine
- Traditional Tibetan medicine













No comments:
Post a Comment